The knee is a complex and crucial joint, essential for our daily mobility and participation in many sports activities. At the heart of this joint lie ligament structures that ensure its stability. Among them, the posterior cruciate ligament, or PCL, plays a fundamental role. Discover what a PCL rupture is, its symptoms, how it is diagnosed, and how it is treated.
What is the Posterior Cruciate Ligament?
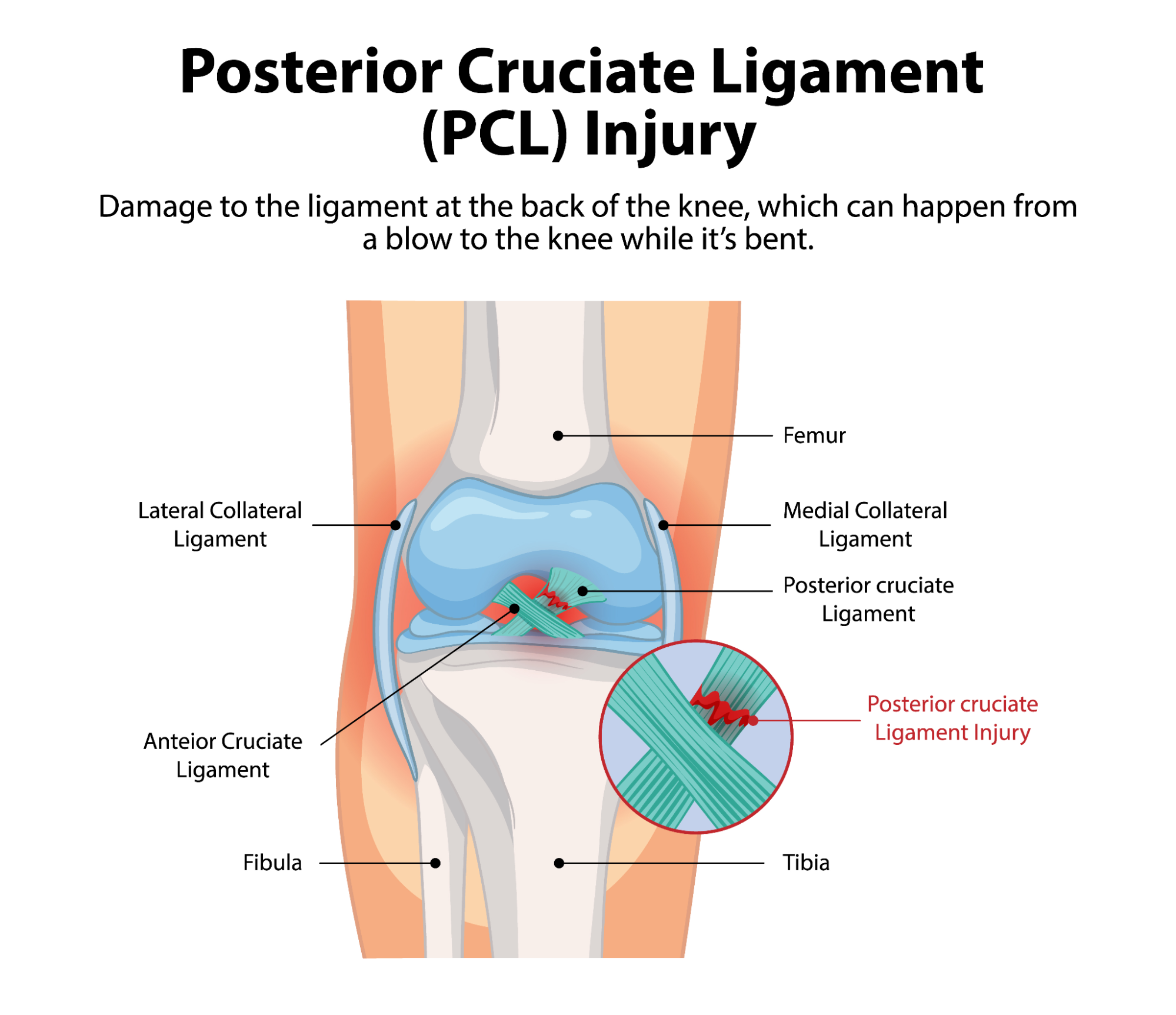
The knee is stabilized by four main ligaments that connect the femur to the tibia, ensuring its proper function and stability. These ligaments include the cruciate ligaments (anterior and posterior) and the collateral ligaments (medial and lateral).
The posterior cruciate ligament or PCL is located in the back and center of the knee. Its primary function is to control the backward movement of the tibia relative to the femur, thus preventing the leg from sliding excessively backward. It is considered the strongest ligament in the knee, making injuries to it relatively rare.
A PCL rupture is a severe injury. It is rarely isolated and is often accompanied by damage to other ligaments or knee structures, such as the menisci or cartilage. The tear can occur at various levels of the ligament, from its upper attachment on the femur to its lower insertion on the tibia.
What Are the Symptoms of a Posterior Cruciate Ligament Tear?
A PCL tear is a traumatic injury that occurs suddenly after an impact. Symptoms can manifest in various ways:
- A popping or cracking sensation, sometimes audible, at the moment of impact,
- Intense and sudden pain at the back of the knee,
- Significant swelling of the joint,
- Difficulty walking,
- A feeling of knee instability, particularly noticeable during braking, descending stairs, or walking downhill. This instability may also be felt during pivoting movements, direction changes, and lateral motions.
During a clinical examination, the doctor may look for a sign called the “posterior drawer.” This test involves bending the leg at 90° and applying backward pressure on the tibia; a backward sliding movement, similar to a drawer, indicates abnormal laxity due to ligament rupture. Signs of impact on the tibia or joint effusion (fluid buildup) may also be present.
Why Is It Painful?
A posterior cruciate ligament rupture is almost always the result of a high-energy, violent impact. These traumas most often occur in the following situations:
- For example, a sudden fall from a bicycle or a motorcycle accident,
- Sports such as football (soccer), rugby, certain combat sports, and sliding sports are frequently associated with this type of injury. One of the most common mechanisms is a direct anterior blow to the upper tibia while the knee is bent at 90°, often called the “dashboard injury.” Other causes include a direct fall onto the knees, landing from a jump with the leg extended, sudden twisting of the knee, or trauma to a straight leg, such as during a rugby tackle. It is important to note that these traumas are not exclusive to PCL ruptures and can also cause other ligament injuries in the knee.
Beyond the initial pain caused by trauma, pain felt after a PCL rupture or surgery is also due to inflammatory reactions in the knee, which can lead to loss of mobility and persistent discomfort, especially during the first days and weeks after surgery.

How Is a Posterior Cruciate Ligament Rupture Diagnosed?
A precise and rapid diagnosis is essential for effective management of a PCL rupture. The diagnostic process typically involves several steps:
-
Clinical Examination:
The doctor performs a thorough knee exam, looking for signs of laxity, as well as bruising or joint effusion.
-
X-rays:
Standard X-rays are taken to rule out any associated fractures or bone avulsions. Dynamic X-rays may be used to objectively measure the posterior drawer and assess the degree of instability.
-
MRI:
MRI is the reference examination to confirm the diagnosis of a posterior cruciate ligament rupture. It provides detailed images that not only confirm the tear but also identify any associated injuries, which are very common and will influence the treatment strategy.
How Long Can the Pain Last?
The duration of pain and recovery after a PCL injury varies considerably depending on the severity of the tear, the need for surgery, and individual patient characteristics.
-
Initial Pain:
After trauma or surgery, pain is common, especially during the first days and weeks. Pain medications are prescribed to manage it, and techniques such as icing are also used.
-
Rehabilitation Duration:
Physiotherapy is essential and can last from 3 to 6 months. If surgery is performed, a specific brace is often worn for 4 to 6 months.
-
Return to Activities:
- Weight-bearing on the operated leg is limited for about the first 6 weeks after surgery.
- Resuming sedentary professional activities is generally allowed from the 4th week post-operation.
- Return to sports activities is a gradual process: cycling and swimming can often be started after 4 weeks of rehabilitation. For running, it typically requires about 5 months, while pivoting sports (involving sudden direction changes) require about 6 months. Sports involving lateral movements, sudden starts, and pivots are generally only allowed around the 8th month after surgery.
These timelines serve as guidelines and are discussed on a case-by-case basis with the surgeon before the procedure. Complete recovery, allowing a return to all previous physical and sports activities, is achieved in the vast majority of cases, but it requires patience and perseverance.

Treatments for the PCL
The treatment strategy for a PCL rupture depends on the severity of the tear, its age, the presence of associated injuries, as well as the patient’s age and level of physical activity.
Non-surgical or Conservative Treatment:
- Most PCL injuries are partial and can heal without surgery. This ligament has a healing potential up to about 6 weeks after the initial trauma.
- Even in cases of complete rupture, surgery is not always mandatory, especially if adequate muscle strengthening can compensate for instability or if the patient’s daily needs do not require it.
- Conservative treatment generally involves:
- Resting the knee for about 6 weeks.
- Pain management.
- A tailored physiotherapy program.
- Wearing a specific brace for about 4 months to promote healing.
- In most cases, these conservative measures provide excellent functional outcomes.
Surgical Treatment or Ligament Reconstruction:
- Surgery is generally necessary for complete tears that cause significant knee instability or in cases of multiple ligament injuries.
- The goal of the surgery is to reconstruct the ligament in its precise anatomical position. The most common technique is ligamentoplasty, which typically utilizes tissue harvested from the patient. For complex or multiple injuries, allografts (tissues from donors) may sometimes be used.
-
Physiotherapy Rehabilitation:
Physiotherapy plays a crucial role in the success of surgery and postoperative healing.
-
Initial Phase:
Rehabilitation starts very early, sometimes as soon as the 5th day after surgery. The goal is to reduce pain and swelling, mobilize the kneecap, and restore full knee extension. It is crucial to activate the quadriceps muscle quickly, the primary stabilizer against the posterior drawer, while avoiding reproducing this laxity movement. Strengthening exercises involving co-contraction of the quadriceps and hamstrings may be performed.
-
Intermediate Phase:
Rehabilitation focuses on regaining the full joint range of motion and progressively strengthening the quadriceps. Hamstring work is integrated cautiously. Scar massages are performed, and activities such as swimming and cycling may be resumed.
-
Advanced Phase:
Muscle strengthening intensifies. Proprioception training is essential for improving balance and knee stability. Functional exercises, such as lunges, squats, and leg presses, are utilized. This is also the phase of re-athletization, where sports-specific technical movements are gradually reintroduced under the supervision of the healthcare professional.
Why Is Consulting a Specialist Important?
Managing a posterior cruciate ligament rupture requires the expertise of healthcare professionals. Consulting a specialist is crucial for several reasons:
-
Accurate and Rapid Diagnosis:
Symptoms of a PCL rupture can be nonspecific, making clinical examination and MRI indispensable for an accurate diagnosis and identification of associated injuries. A quick diagnosis is essential for proper healing.
-
Personalized Treatment Plan:
An orthopedic surgeon or sports medicine physician will evaluate the severity of the injury, its age, and the patient’s goals to determine the most appropriate treatment, whether conservative or surgical.
-
Specialized and Supervised Rehabilitation:
Physiotherapy after a PCL rupture is systematic and fundamental for recovery. A physiotherapy specialist, such as a physician at AMS Clinics, will guide the patient through the different rehabilitation phases. They will tailor exercises to relieve pain, restore mobility, and rebuild muscle strength and knee proprioception. Early management is essential for optimal results. Pre-operative rehabilitation may even be prescribed to prepare the knee for surgery or, in some cases, to try to avoid it.
-
Optimizing Return to Activities:
The specialist will support the patient until they can return to daily and sporting activities safely, validating each step of the recovery process.

Conclusion
Being supported by a medical team ensures comprehensive and individualized care for posterior cruciate ligament pain. This approach maximizes the chances of complete healing and an optimal return to an active life. With the AMS Clinics team, you have access to a comprehensive medical team specialized in managing knee pain and ligament ruptures.


Recent Comments