Vertigo is a disorienting sensation that can severely impact quality of life, causing anxiety and limiting daily activities. Among its many causes, Benign Paroxysmal Positional Vertigo (BPPV) is the most common. Although often frightening, BPPV is generally benign and, most importantly, highly treatable. This article explores what BPPV is, its causes, symptoms, and the effective treatment options available, primarily through physiotherapy, to help restore balance and well-being.
What is BPPV?
The term vertigo comes from the Latin vertere (“to turn”), referring to an intense spinning sensation. BPPV is characterized by brief, sudden episodes of rotational vertigo, where you feel as though you or your surroundings are spinning. This differs from dizziness, which feels more like imbalance or lightheadedness.
BPPV is a vestibular disorder linked to the inner ear’s balance system. It occurs when tiny calcium carbonate crystals, called otoconia or otoliths, detach from their normal location in the utricle and move into the semicircular canals that regulate balance. When the head moves into certain positions (looking up, lying down, or rolling in bed), these floating crystals shift in the fluid of the canals, abnormally stimulating nerve receptors. This sends false signals to the brain, creating the illusion of motion.
Other Common Causes of Vertigo
While BPPV is the most frequent cause, other conditions may also trigger vertigo:
- Acute labyrinthitis: viral infection with sudden symptoms.
- Ménière’s disease: recurrent vertigo lasting 2–24 hours, often with hearing loss.
- Vascular vertigo: caused by poor blood circulation.
- Post-traumatic vertigo: following a head injury.
- Peripheral vestibular disorders: inner ear issues.
- Central neurological disorders: affecting the central nervous system.
A professional evaluation by a healthcare provider, such as a physiotherapist, is essential to identify the exact cause and recommend proper treatment.
How Common is BPPV?
BPPV is the leading cause of vertigo, accounting for 25–35% of all vertigo cases and 60% of peripheral vertigo cases. About 2.4% of people will experience BPPV at some point in their lives.
- It mainly affects older adults, peaking around age 50.
- Women are more frequently affected (about 64% of cases).
- It is rare before age 35, except after head trauma.
Symptoms of BPPV
Typical signs include:
- Sudden, intense spinning vertigo.
- Short episodes, usually lasting less than one minute.
- Triggered by head position changes (getting up, lying down, turning in bed, looking up).
- Often worse in the morning.
- Frequently associated with nausea, sometimes vomiting.
- Temporary difficulty maintaining balance after an episode.
- No hearing loss or tinnitus (if present, other causes must be considered).
Types of BPPV
BPPV is classified by the affected semicircular canal:
- Posterior canal BPPV: most common (≈90% of cases).
- Horizontal canal BPPV: 5–10% of cases; often triggered when turning the head sideways while lying down, and may last longer.
- Superior (anterior) canal BPPV: rare (≈1% of cases), often more intense and more challenging to diagnose/treat.
How is BPPV Diagnosed?
Diagnosis is primarily clinical, based on symptoms and physical examination. Key diagnostic maneuvers include:
- Dix-Hallpike test: gold standard for posterior and superior canal BPPV. Patient is quickly moved from sitting to lying with the head turned 45° and tilted back. Vertigo and eye movement (nystagmus) confirm diagnosis (over 90% accuracy).
- Head-hanging maneuver: used for anterior canal BPPV, observing downward nystagmus.
- Lempert (roll) test: used for horizontal canal BPPV, involving a 360° head/body rotation.
These maneuvers may trigger vertigo but are critical for pinpointing the canal involved. Additional tests (audiogram, VNG, vHIT, VEMP, MRI) may be required if symptoms are atypical or persistent.
Treatment and Relief Options
1- Vestibular Physiotherapy (Primary Treatment)
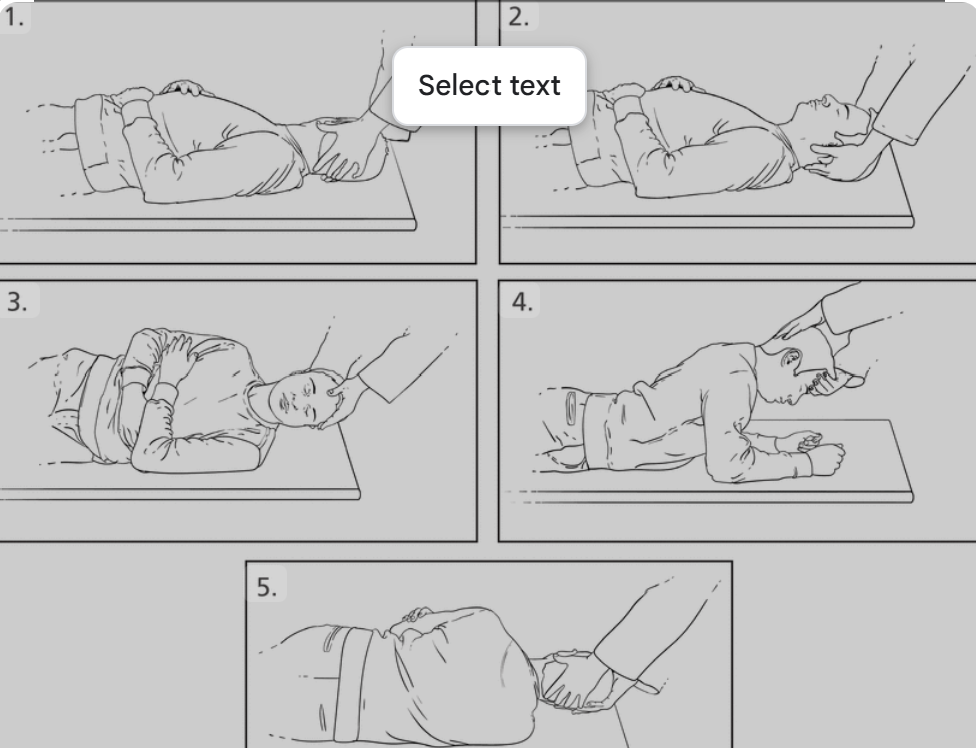
Vestibular rehabilitation is the most effective therapy for BPPV. Physiotherapists trained in this field guide repositioning maneuvers to restore balance.
- Repositioning maneuvers: move the crystals back to the utricle for absorption.
- Epley maneuver: very effective for posterior canal BPPV (80–100% success).
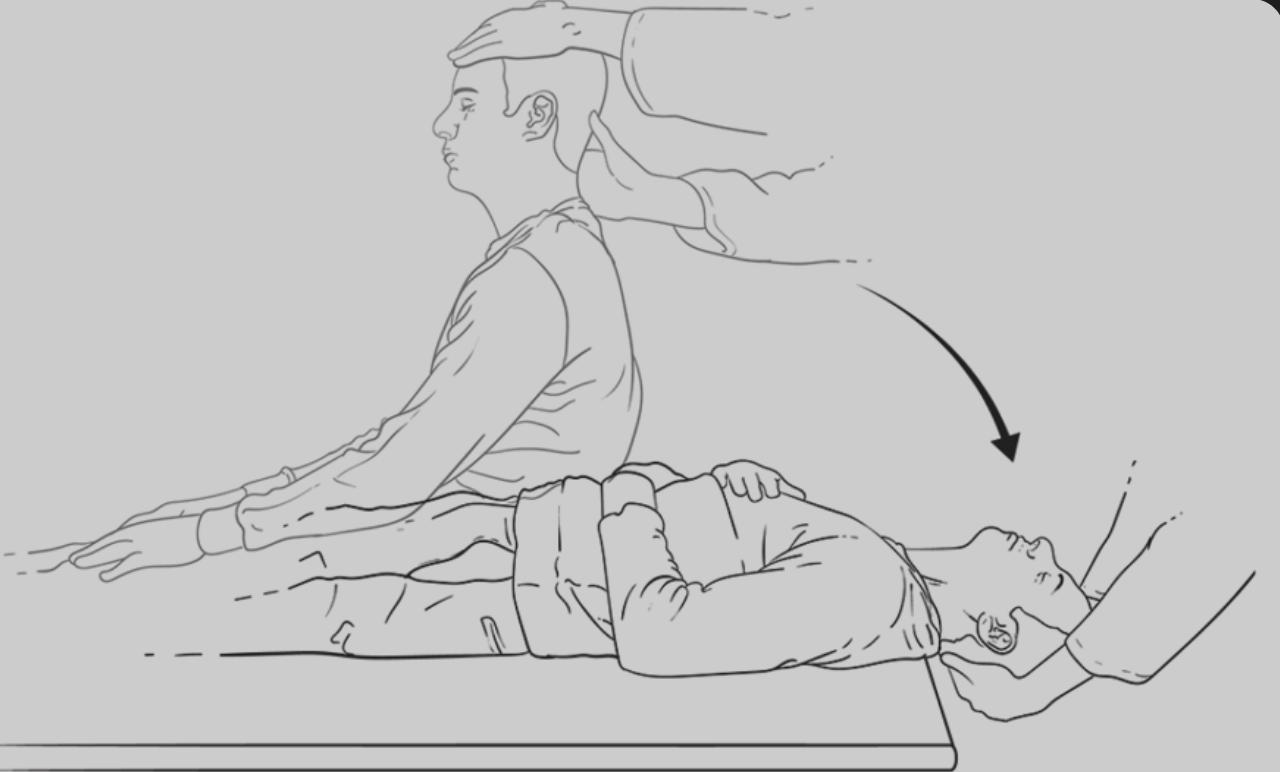
- Semont maneuver: an alternative for posterior canal cases.
- Lempert maneuver: for horizontal canal BPPV.
- Head-hanging/Yacovino maneuver: for anterior canal.
👉 Many patients recover immediately. Some require several sessions. Overall cure rates exceed 80–90%.
- Rehabilitation programs typically last from 3 to 10 weeks, with an average of 3 sessions. Exercises may initially reproduce vertigo, but are essential for progress.
- At-home exercises: taught by physiotherapists for daily practice.
- Holistic approach: also addresses anxiety, muscle tension, and avoidance behaviors.
(Fun fact: Vestibular rehab techniques were initially developed by NASA to help astronauts adapt to weightlessness!)
2- Medical and Complementary Approaches
- Vitamin D supplementation is recommended in cases of deficiency to reduce recurrence.
- Avoiding sudden head movements: short-term advice while retraining balance.
- Surgery (rare): considered only in severe, resistant cases. Posterior canal occlusion surgery is highly effective (>90% success) but carries the risk of hearing loss.
Conclusion
Though distressing, BPPV is a benign and fully treatable condition. Early diagnosis and proper management are key to regaining balance and confidence.
- Physiotherapy and vestibular rehabilitation offer safe, highly effective relief.
- Most patients see improvement within 1 day to 3 weeks.
- Success rates exceed 80%, rising above 90% with repeated maneuvers.
However, some conditions like Ménière’s disease respond less well and require alternative management.



Recent Comments