A Colles’ fracture is a widespread wrist injury that can significantly affect daily activities and quality of life. Often linked to a fall, it involves a break in the radius bone near the wrist. Understanding this injury and the available treatment options is essential for lasting relief.
What Is a Colles’ Fracture?
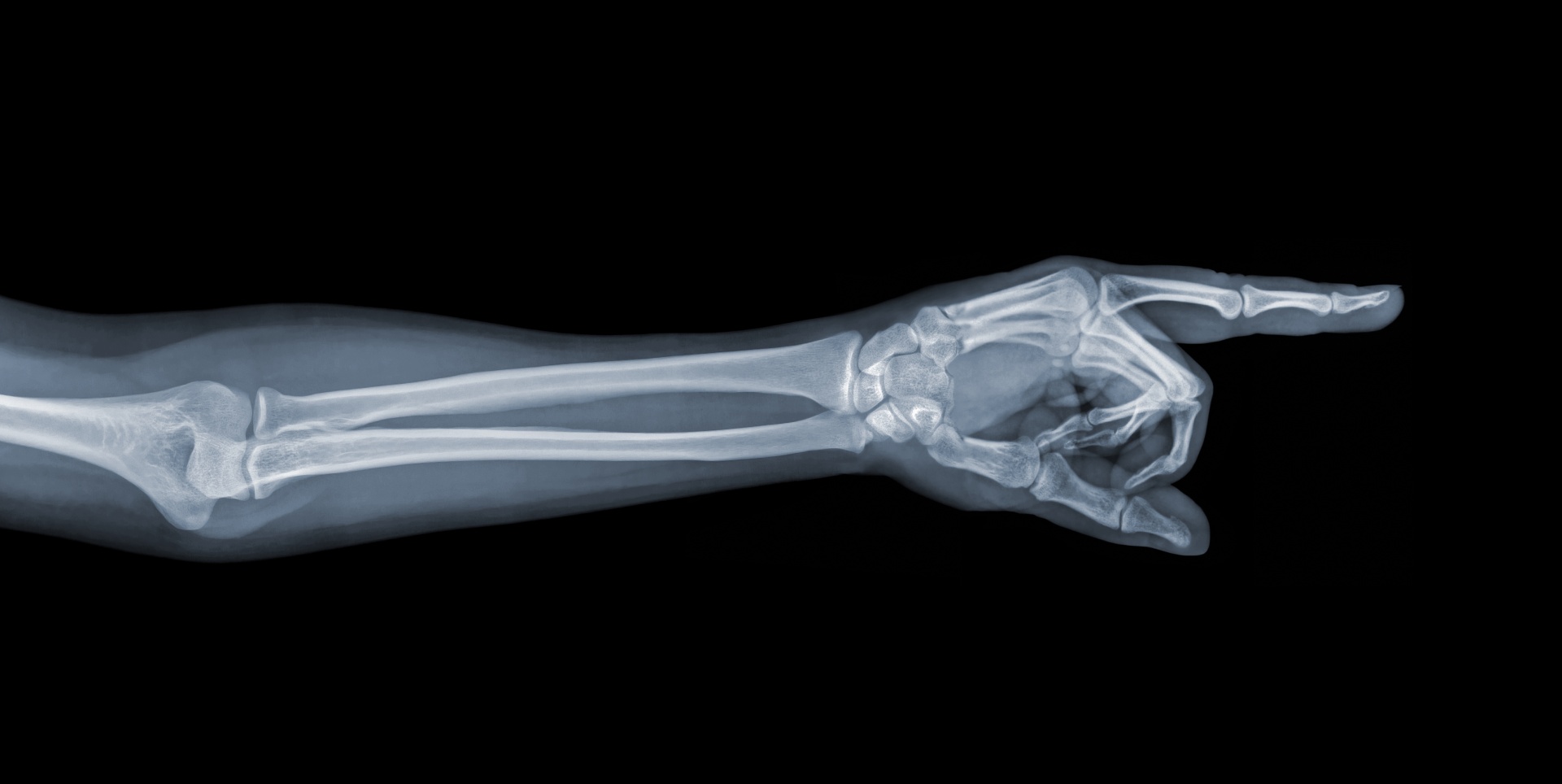
First described in 1814 by Abraham Colles, a Colles’ fracture is a break in the distal radius, one of the two forearm bones. It is considered an extra-articular fracture, meaning it does not directly involve the wrist joint, but it causes a characteristic displacement of the bone fragment.
The fractured segment is tilted and displaced toward the back of the hand and toward the thumb side.
This visible deformity is often called the “dinner fork deformity” due to its appearance.
The wrist is made up of several bones: the radius, ulna, and eight carpal bones. A Colles’ fracture is the most common type of distal radius fracture.
Less frequently, if the wrist is bent forward during the fall, the bone may be displaced in the opposite direction. This is called a Smith’s fracture (or Goyrand-Smith fracture).
Causes
The primary cause is a fall onto an outstretched hand, with the wrist in extension and radial deviation. It’s a natural reflex to break a fall.
This fracture is prevalent among:
- Postmenopausal women and seniors: osteoporosis weakens the bones, raising fracture risk to nearly 20% after age 65.
- Young active adults or athletes: usually linked to high-energy trauma, such as sports injuries or motor vehicle accidents.
- Children and adolescents: their developing bones are less dense, making them more vulnerable.
Bone fragility, mainly due to osteoporosis, is a significant risk factor.
Symptoms
Typical signs of a Colles’ fracture include:
- Sudden, intense pain in the wrist and fingers.
- Pronounced swelling and tenderness.
- A visible or palpable deformity of the wrist (dinner fork appearance), sometimes with outward or bayonet deviation.
- Inability to move the wrist and forearm.
- Possible bruising (hematoma).
- If the median nerve is involved, numbness in the index fingertip and difficulty opposing the thumb and little finger.
Patients often present holding the injured wrist with their other hand.

How Long Does Recovery Take?
Recovery varies, but early diagnosis and treatment are crucial for good outcomes.
Without appropriate care, complications can include:
- Stiffness and loss of wrist/finger mobility.
- Persistent chronic pain or wrist osteoarthritis (especially if the fracture involves the joint or has significant displacement).
- Peripheral neuropathy, particularly median nerve compression (carpal tunnel syndrome).
- Complex regional pain syndrome (CRPS) can complicate healing.
- Tendon rupture.
- Shoulder stiffness (“frozen shoulder”) from prolonged arm immobilization.
Most functional recovery occurs within 6 months, but more minor improvements may continue for up to 4 years, highlighting the importance of early rehabilitation.
Treatment Options
Treatment depends on fracture severity, displacement, and patient age. The main goal is to restore proper bone and joint alignment and maintain it to prevent further displacement.
1. Conservative treatments
- Reduction and immobilization: bones are realigned without surgery (closed reduction), often under local or general anesthesia. The wrist is then immobilized in a cast or splint for 4–6 weeks.
- Pain and swelling management: ice, analgesics, and elevating the hand are common.
- Finger mobilization: moving the fingers and elbow daily during immobilization helps prevent stiffness.
- Orthoses: thermoformable orthoses can help post-surgery with hygiene and scar care.
2. Surgical treatments
Surgery may be needed if:
- Conservative care fails after several months.
- The fracture has significant displacement.
- The joint is involved.
- Bones are impacted or stuck.
Surgical techniques include fixation with plates, pins, or external fixators (a metal frame with pins inserted into the bone). External fixation may be temporary before further surgery.
Post-surgical rehab: physiotherapy begins within days to prevent adhesions and restore muscle strength. Rehab usually lasts 3–6 months.
Physiotherapy: A Path to Recovery
Physiotherapy is essential after a Colles’ fracture, whether treated conservatively or surgically. Outcomes are best when started early.
How physiotherapy helps:
- Pain and swelling reduction: electrotherapy (TENS), contrast baths, ice, paraffin baths, plus education on pain and edema control.
- Restoring mobility: joint mobilizations, soft tissue techniques, and prescribed active, assisted, and passive exercises (flexion, extension, pronation, supination).
- Strengthening: progressive exercises for the rotator cuff, wrist, and hand muscles to stabilize the arm and restore function.
- Functional return: exercises simulating daily tasks (e.g., unscrewing a lid, buttoning clothes) and guidance for safe return to work and activities.
Conclusion
A Colles’ fracture is a frequent wrist injury that requires timely, appropriate care. Whether managed conservatively or surgically, a personalized plan that includes physiotherapy is key to regaining full, pain-free wrist function.


Recent Comments